
MedsDental ensures every patient’s dental insurance is verified accurately. Our expert team reduces claim denials, prevents payment delays, and protects your practice revenue. Let our team handle verification so your staff can concentrate on patients.

These are common mistakes that can lead to verification failures:
Every step of insurance verification is managed accurately, keeping your practice on track and your revenue protected.

Skipping this step can lead to major issues, including delayed payments and unsatisfied patients. Here’s why verification should never be skipped:

Ensures accurate billing and avoids submitting claims for non-covered services.

Patients are fully informed about what’s covered and what’s not.

Helps patients understand deductibles, copays, and coverage limits.

Keeps your front desk organized and billing teams proactive.
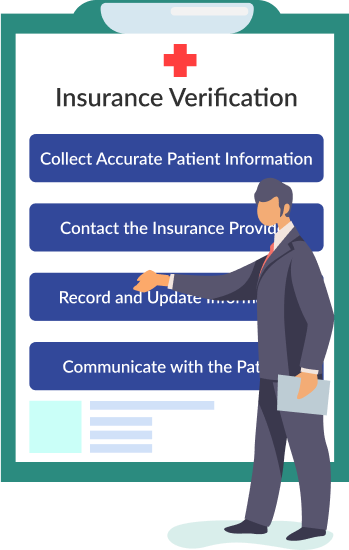
We manage the entire insurance verification process so your staff can focus on patients.
Collect Patient Information
We gather and verify all essential details including full name, date of birth, insurance ID, employer information, and provider before the first visit.
Verify Coverage with Insurance Providers
Our team confirms coverage, policy dates, services included, deductibles, copays, waiting periods, and annual limits directly with the insurer.
Record and Update Information
All details are documented in the patient file and your practice management system, with a verification log maintained for reference.
Communicate Coverage to Patients
MedsDental informs patients about plan coverage, exclusions, and expected costs before appointments to reduce surprises and improve satisfaction.

Even when processes are in place, these issues often occur:
Long Hold Times
Insurance companies can be slow to respond
Outdated Information
Patients may not know about policy changes.
Human Error
Miscommunication between staff and providers can lead to wrong entries.
Last-Minute Verifications
Waiting until the appointment day can create chaos.
Dental process authority to fetch information directly from EHR system
Insurance verification can take hours and impact your practice revenue. MedsDental manages the entire process by confirming coverage, benefits, and deductibles. Your staff can focus on patients while we reduce denials, speed up reimbursements, and protect collections.
Practice Management Software:
We work with Dentrix, Eaglesoft, OpenDental, and other platforms to access patient records and insurance information.
Eligibility Verification Services:
Using RCM (Revenue Cycle Management) solutions, we confirm coverage, deductibles, and benefits before treatment.
Clearinghouses:
We connect with providers like Change Healthcare or Vyne for smooth claim submission and verification.
With MedsDental’s insurance verification, practices see faster payments, higher collections, and improved patient satisfaction:

MedsDental handles preauthorizations so your practice knows exactly what each patient’s plan covers before treatment. Avoid denied claims, unexpected costs, and delays while keeping patients informed.
With our service, you can:
● Confirm coverage for every procedure in advance
● Reduce claim denials and lost revenue
● Give patients clear cost expectations
● Stay compliant with insurance rules and regulations
Let us manage preauthorizations so your team can focus on care while your revenue stays protected.
Avoid the frustration of collecting additional payments that fall between an estimated co-pay and what an insurance policy covers. An angry patient is far less likely to pay because they feel betrayed and tricked. Using the MedsDental platform to help you verify your patients’ insurance up front, you significantly reduce this issues in your practice and save thousands each year!
Having updated and accurate insurance information on file for your patients means you can provide accurate treatment plans and better estimated costs to your patients. This decreases the likelihood of a patient having an outstanding balance when the insurance company has paid its share. Keep your patients happy and your accounts receivabe low with the better insurance verification!
We don’t have to tell you that when a patient is happy your practice is profitable. Balances are paid, no-show appointments are reduced, and patient referrals flood in. Eliminate the unpleasantness of having to tell a patient they owe you far more than you quoted them.
It’s the process of confirming a patient’s dental benefits and eligibility with their insurance provider.
Government programs such as Medicare have their provider enrollment, chain, and ownership system (PECOS). The approval of provider enrollment and provider credentialing in medical billing is faster than commercial insurance providers, and Medicare has an average approval time of 41 days. On the other hand, commercial insurance carriers can take anywhere from 60 to 180 days. Therefore, this is a game of waiting, hurrying, and waiting again.
Timely arrangements of the required documents, e.g., malpractice, DEA, state license, and various other documents, with the utmost efforts of initial research with every state payer to have everything ready before filing the new credentialing applications.
The first and foremost thing is to initiate applications with available IPAs to get contracted in the first place. Otherwise, we can escalate/expedite our request to join the network with payers in the form of appeals.
Full name, DOB, insurance ID number, group number (if applicable), and provider name.
Dental insurance verification isn’t just an administrative task—it’s a strategic process that helps practices reduce losses, improve cash flow, and give patients a smoother experience.
Want help verifying dental insurance or managing your billing more efficiently? Contact us for professional RCM and verification services customized for dental practices.
Let’s Connect
© MedsDental. All rights reserved 2026. Powered by MeshSq.



